The intestinal microbiota influences stress and cognitive performance
This article supports our protocol for the treatment of children with symptoms of attention deficit with pronounced hyperactivity, autistic features, or with moderate to severe autism.
The source of the article is available in its original and complete version here : https://academic.oup.com/nutritionreviews/article/73/suppl_1/28/1819270
INTRODUCTION
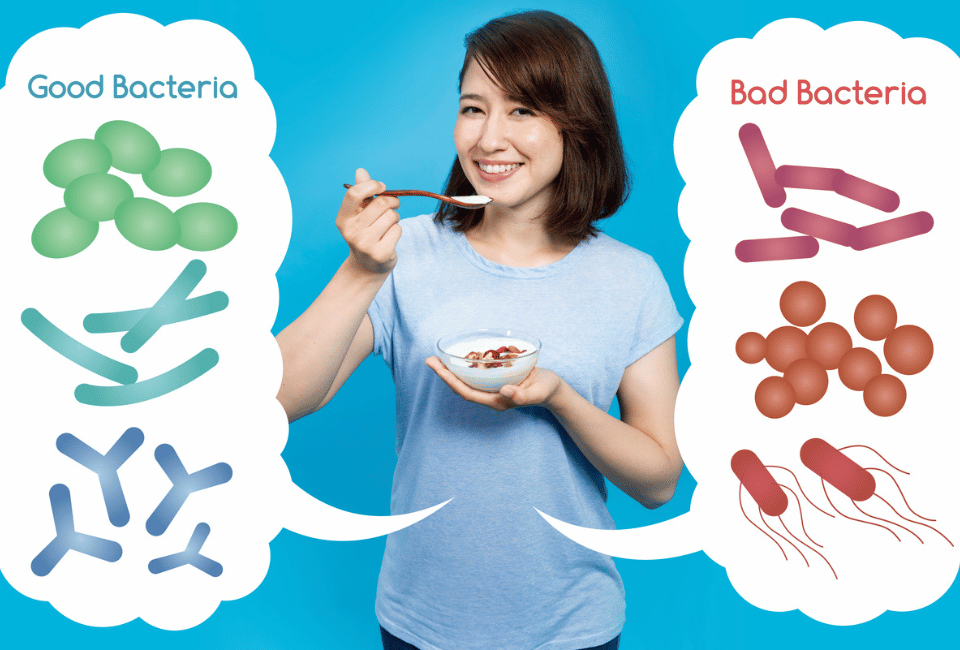
The gut microbiota is composed of trillions of microbes that influence normal physiology and alter the host’s susceptibility to disease.1 A growing body of evidence in animals supports the concept that the gut microbiota influences emotional behavior.2–6 Changes in the gut microbiota or intestinal exposure to specific bacteria can modulate the peripheral and central nervous systems (CNS) in animals, resulting in altered brain functioning and suggesting the existence of a microbiota gut–brain axis.7 There is good evidence from animal studies that gut bacteria influence brain chemistry and development and that the enteric nervous system, including the sensory vagus nerve, appears to be able to differentiate between nonpathogenic and potentially pathogenic bacteria7 and may play a critical role in mediating the effects of gut microorganisms on behavior.7,8 Because the nervous system has constant bidirectional communication with the immune system, the effects of bacteria on the nervous system cannot be disassociated from effects on the immune system. This type of crosstalk occurs regularly and can have profound neurological and immunological effects. However, the exact molecules responsible for host–microbe communication remain largely unknown.9 Studies are currently addressing this neural circuitry and investigating the extent of the influence of gut microbiota on the CNS and on behavior,7 as well as the therapeutic potential of probiotics for a range of immune disorders.10 Microbiota products and metabolites also may promote metabolic benefits such as reduced body weight, reduced adiposity, improved glucose control, and improved insulin sensitivity via gut–brain neural circuits.11
PROBIOTICS AND HEALTH
While the composition of the gut microbiota varies greatly among individuals, alterations to the balance of common gut microbes may affect production of the short-chain fatty acids (SCFAs), butyrate, propionate, and acetate, which are products of intestinal bacterial fermentation that regulate intestinal adaptive immune responses12 and play key roles in CNS function.11,13,14 Butyrate has direct effects on the growth, maturation, and functioning of gut epithelial cells,13 on Treg cells of the immune system (regulatory T cells that play a key role in preventing autoimmunity), and on the nervous system, inhibiting IKca (an intermediate conductance Ca activated K+ channel).15
Germ-free mice have reduced concentrations of SCFAs compared with normal animals.12 Smith et al.12 fed germ-free mice SCFAs for 3 weeks and found that individual SCFAs or a combination of SCFAs increased immunoregulatory Treg cells. Ochoa-Reparaz et al.16,17 found that Bacteroides fragilis or its exopolysaccharide, polysaccharide A (PSA), given to mice in experimental autoimmune encephalomyelitis models protected against CNS demyelinating disease both prophylactically and therapeutically.
A recent study also found that SCFAs, especially butyrate, positively influenced host metabolism by activating intestinal gluconeogenesis, both in insulin-sensitive and insulin-insensitive states, promoting glucose and energy homeostasis.11 Diets high in nondigestible carbohydrates lower the pH in the proximal colon, which may be an important factor in butyrate production.13 Propionate and acetate also have been found to promote satiety.18 The metabolic benefits on body weight and glucose control induced by SCFAs or dietary fiber in normal mice are absent in mice deficient for intestinal gluconeogenesis, despite similar modifications in gut microbiota composition.11 This finding suggests that while diet is a major factor in determining the composition of the gut microbiota and the production of SCFAs in mice, there is a strong interaction with genotype that influences outcomes.11
Altered gut microbiota can also be responsible for pathophysiology in the colon.19,20 Gut microbiota–host misadaptation (dysbiosis) has been implicated in the rising incidence of inflammatory diseases such as inflammatory bowel disease.1 Patients with inflammatory bowel disease or irritable bowel syndrome experience reduced levels of Lactobacillus and Bifidobacterium species in the gut.19,20 Animal models indicate a role for bacteria in the adequacy of immune regulation and the development of intestinal inflammation. It is likely that reduced numbers and diversity of normal beneficial commensals such as lactobacilli and bifidobacteria play an important role in allowing detrimental microbes such as Citrobacter rodentium and Escherichia coli access to the epithelial surface.21 Disease improvement occurs following manipulation of the gut microbiota with Lactobacillus rhamnosus and Lactobacillus helveticus probiotics.21 Animals administered B. fragilis or even PSA, which initiates beneficial immune responses, can be protected from experimental colitis.9 Probiotics can also improve gut dysfunction induced by stress, in part, by normalization of hypothalamic–pituitary–adrenal axis (HPA) activity.21
PROBIOTICS AND BEHAVIOR
The HPA reaction to stress is programmed in early life (at least in rodents). A landmark study from Japan demonstrated that early exposure to gut microbiota reduces the exaggerated HPA responses of germ-free mice in adulthood but not if given to adult animals.22 Plasma ACTH and corticosterone levels were greater in response to stress in germ-free mice compared with specific pathogen-free mice.22 Studies have shown similar results in normal, healthy mice and rats, i.e., that feeding a probiotic can attenuate the HPA axis response to stress.15,23,24 Finally, it is important to recognize that stress itself has a major consequence on the composition and function of the gut microbiota.25
Mice fed L. rhamnosus JB-1 for 28 days experienced changes in certain Gamma amino butyric acid (GABA) receptors in different regions of the brain, increased anxiolytic behavior, and inhibition of corticosterone response to acute stress.23 These changes were compatible with benzodiazepine effects. The neurochemical and behavioral effects were not found, however, in vagotomized animals, indicating that the vagus nerve is a major communication pathway between such bacteria in the gut and the brain.23 Screening for this type of enteric nervous system activity could possibly provide potential treatments for anxiety and stress.
Recent unpublished research shows that the amount of the neurotransmitters GABA and glutamate can be increased in the brain by feeding the same probiotic bacteria to animals. However, the effects are limited, are time dependent, and depend on the continued presence of the starting probiotic.
It also has been demonstrated that when animals are fed L. rhamnosus, effects can be seen not only on the local nervous system but systemically as well.26 Indeed, the intestinal microbiota can clearly influence brain chemistry and behavior in mice independent of the autonomic nervous system, gastrointestinal-specific neurotransmitters, or inflammation.27 Fecal transplants from specific pathogen-free NIH Swiss mice, which are relatively not anxious, to BALB/c mice, which are relatively anxious, surprisingly showed that the behavior of the animals was dependent on the source of fecal/microbiota material. Colonization of germ-free BALB/c mice with microbiota from NIH Swiss mice increased exploratory behavior, suggesting reduced anxiety, and increased hippocampal levels of brain-derived neurotrophic factor, which is important for the growth, differentiation, and maturation of neurons. In turn, colonization of germ-free NIH Swiss mice with BALB/c microbiota reduced exploratory behavior, suggesting an increase in anxiety. These changes were unaffected by vagotomy.
Diet can also change the profile of gut microbiota and, thereby, host behavior. Li et al.28 showed that changing the composition of the diet of rodents altered the spatial memory of the recipients, indicating that nutrition and diet must be taken into account in such studies.
Research with a mutant bacteria devoid of PSA suggests that this component is necessary and sufficient for acute activation of intestinal sensory neurons, i.e., PSA can mimic the effects of the parent organism on the nervous system, much as it can mimic its immunological effects.9,29 Thus, components of bacteria may themselves have the capacity to affect the functions of the nervous system. These findings support the concept that the luminal content of the gut and the bacteria contained within are important factors in determining behavior and even cognition in animals.27
HUMAN RESEARCH
The strong evidence in animals of a direct link between the gut microbiota and the brain has led to the suggestion that the effect might be similar in humans. Bercik et al.27 suggested that intestinal dysbiosis might contribute to psychiatric disorders in patients with bowel disorders. However, to date, there has been very little evidence in humans that probiotics will have the same neurochemical and behavioral effects observed in animals. In a double-blind, randomized, placebo-controlled study, Messaoudi et al.30 administered a probiotic formula (L. helveticus and Bifidobacerium longum) to healthy women for 30 days and then assessed the recipients’ level of anxiety and depression and 24-h urinary-free cortisol levels. In the female volunteers, daily administration of the probiotic formula alleviated psychological distress as indicated in 3 behavioral assessments, and 24-h urinary cortisol was reduced in the treated women.
In another clinical pilot study, 39 patients with a diagnosis of chronic fatigue syndrome were randomly assigned to receive Lactobacillus casei Shirota or a placebo daily for 2 months. There was a significant decrease in anxiety symptoms in the treated group.31 A more recent clinical study was performed in 23 healthy women volunteers with no gastrointestinal or psychiatric symptoms. The women were randomly assigned to groups given either a fermented milk product (Bifidobacterium animalis, Streptococcus thermophilus, L. bulgaricus, and Lactococcus lactis) or a placebo, which consisted of a nonfermented milk product adjusted for taste and texture, twice daily for 4 weeks.32 Consumption of the fermented milk product had a robust effect on activity of the brain regions that control central processing of emotion and sensation, as observed with functional magnetic resonance imaging before and after consumption of the fermented milk product.
Some individuals diagnosed with autism spectrum disorders also display a spectrum of gastrointestinal abnormalities.33 A recent study examined an animal model for the neurodevelopment disorders of autism in which pregnant mice were injected with a viral mimic (POLY I:C). This produced typical stereotypical autistic behaviors in the offspring that lasted into adulthood. Oral administration of B. fragilis to pregnant mice before and immediately after birth resulted in the development of significantly diminished autistic behaviors.33 In this model, the administration of PSA did not prevent all of the abnormalities. However, the findings suggest that the incidence of viral infection over the course of pregnancy may produce lasting effects, which are potentially reversible by the oral administration of particular bacteria.
The findings of these clinical studies are consistent with the findings in rats and mice and suggest that the communication between gut microbiota and the brain is modifiable and may provide targets for the treatment of patients with heightened stress responses associated with gut dysbiosis.32
CONCLUSION
The changes that occur in the microbial content of the gut as a result of ingestion of probiotic bacteria or changing the balance of gut microbiota in other ways can trigger a variety of mechanisms. These include effects on the host immune, nervous, and endocrine systems, which in turn affect each other, demonstrating an important role of the crosstalk between the gut and the host. Behavior, mood, and the response to stress can all be affected by the ingestion of probiotic bacteria. These data are very exciting and have aroused great popular and scientific interest. There is currently a significant gap between the experimental and clinical data. The challenge now is to translate these animal findings into clinical application. In the future, the composition, diversity, and function of specific probiotics, coupled with more detailed knowledge of the composition of gut microbiota, could potentially help in developing more effective diet and drug therapies.